“What gets measured, gets managed.” What If I told you, “what gets measured, could be measured and managed in real-time?” On your wrist.
If you’ve been diagnosed with Type 2 diabetes like me, I’m going to take you on a deep dive into a device that is a game changer: the Continuous Glucose Monitor.
While I have no aversion to needles, many people do. And having to poke your finger every morning to draw blood and check your fasting blood glucose levels, then potentially doing the same thing throughout the day, can be anxiety inducing. Today, we know a lot more about diabetes and it isn’t as simple as someone overeating, or having too much sugar or processed foods in their diet. The cause may be genetic and a Continuous Glucose Monitor could be the difference between someone learning to manage their affliction, or that affliction progressing to the point where they need insulin injections, or worse, amputations or death from comorbidities.
If you’re an iPhone or Apple Watch user, here’s how you can get the most out of a Continuous Glucose Monitor — and which ones get the job done best.
What is a Continuous Glucose Monitor?
I’ll refer to a Continuous Glucose Monitor as a CGM from here on out. For most diabetics, we’ve had to use a Blood Glucose Meter which requires you to use a lancet to poke your finger until it bleeds, drawing blood from your capillaries, so that you can put a drop of it on a ‘stick’ which is then inserted into your meter to give you a blood glucose reading. This is the most accurate way to measure blood glucose (BG).
The FDA says continuous glucose monitoring is accurate enough for commercial use and safe enough to give you an estimation of your current or trending blood glucose levels.
A CGM is often a system which includes a small disk which has a filament on its underside which gets inserted just below the skin and measures the glucose (“sugar”) content in your skin’s interstitial fluid. Interstitial fluid is a thin layer of fluid which surrounds the body’s cells and gets its nutrients from the body’s blood capillaries. Interstitial fluid makes up about 40% of the water in your body. With current technology, that disk with the filament can stay on your body anywhere from 7 to 14 days. There’s even one CGM which gets surgically inserted under your skin by a medical professional and lasts for six months. Though not as accurate as the age-old finger poke, the deviation is plus or minus ~8%, and so the FDA says continuous glucose monitoring is accurate enough for commercial use and safe enough to give you an estimation of your current or trending blood glucose levels. That comes with some caveats I’ll address near the end of the article when we talk about apps.
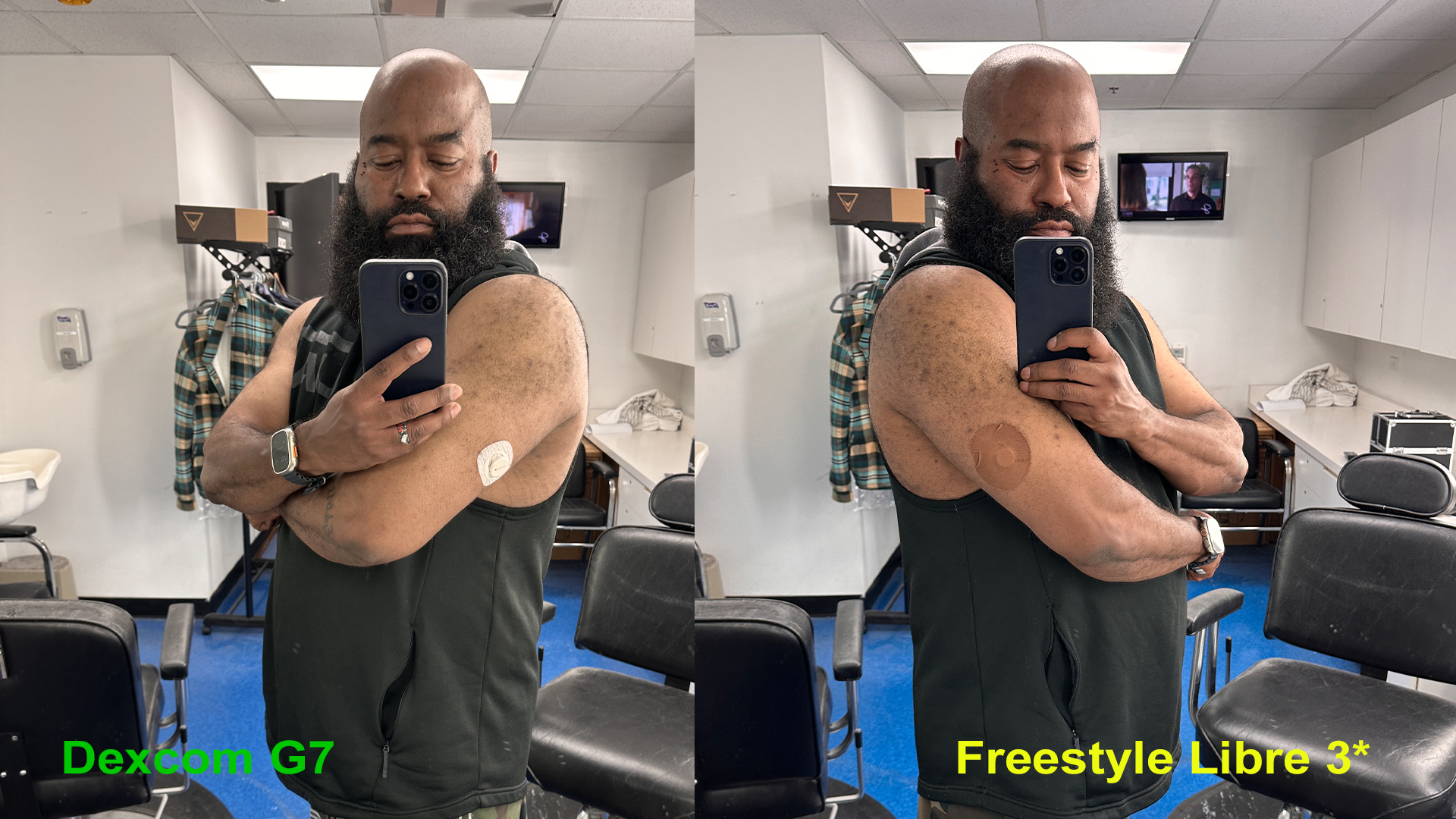
The CGMs available today all connect to your iPhone (or Android device) via Bluetooth and transmit readings back at varying frequencies. For this article I’m looking at two specific CGMs. For 10 days, I wore the Dexcom G7 on the backside of my right arm, and Abbott’s Freestyle Libre 3 on the backside of my left arm.
I didn’t take on Medtronics’ Guardian Sensor 3 because going through its materials it seemed to be the most laborious in terms of application, and it involved the use of the word “needle” which may be off-putting to some users scared of needles — and somewhat defeats the appeal of a CGM. Another option is the Eversense E3 CGM, and it must be surgically inserted under the skin, and removed/replaced by a medical professional every six months. This sensor also requires a separate transmitter to be placed on your arm, though it is removable. The E3 is the only sensor that actually has haptics on board which will vibrate to give you low and high blood glucose warnings, no phone app required. They call this feature “body vibes.” I’m not a huge fan of any medical instrument which is not medically necessary being inserted into my body and living there for six months, so I passed on this one. For now, at least.
Dexcom G7 vs Abbott’s Freestyle Libre 3
Let’s talk about the two I used. When I’ve spoken to medical professionals I know personally, these seem to be the two most common products prescribed by doctors. I’ve actually been a user of Abbott’s previous generation of Freestyle devices, their 14 day Freestyle Libre 2 sensors, and found them to be an amazing tool in managing my Type 2 diabetes. Those are still available for prescription if your provider doesn’t offer the next gen unit. I was looking forward to using the new Freestyle Libre 3 and seeing how it improved on the 2.
To begin with, the 3 is the size of two pennies stacked where the 2 is the size of two quarters. The sensor in the 3 transmits data to your iPhone every minute, as long as it’s within 33 feet of the sensor. You’ll get a nasty nag alarm letting you know when you’re out of range. This sensor is water-resistant up to 1 meter/3 feet of water for no longer than 30 minutes. The Libre 3 is even easier to apply than the 2, which had a two piece applicator. The Libre 3 now has a one piece applicator, where you just twist the top off the unit, then apply the sensor to your body.
The package comes only with the sensor, but for many people I’d suggest picking up an adhesive cover like the Skin Grip Chocolate one I’m wearing in the picture above on the right. Especially for my melanated readers for whom the white sensor may stand out more against your flesh, if you care about being discreet. This brand is available for Libre, Dexcom and Medtronic units, in 10 different color varieties, including tan and clear. I’ve also bumped a sensor, dislodging it, which kills it — and at $38 a pop, WITH insurance coverage, that’s a loss twice a month I don’t want to pay for. So I found those skin tone protective covers on Amazon and bought the variant specifically for the Libre 2 (but the Libre 3 being smaller, they’ve worked just fine for that model too). Additionally, with both of these sensors, you can buy third-party patches like mine which claim to be waterproof. I haven’t tested that claim by jumping into the ocean or a swimming pool just yet but summer is upon us and I’ll report back via my Twitter account if I do.

Now the Dexcom G7 sensor is a bit larger than the Libre 3, but features a one-piece applicator like the Libre 3. Unlike the Libre 3, the G7’s applicator requires that you only press it against the back of your upper arm, then press a button and the applicator does the rest. You then push on the sensor for 10 seconds to be sure it’s seated. Also, unlike the Libre 3, the G7 comes with a protective cover in the box. Not as rugged, I think, as the one I bought third party though. We’ll see over time how it stands up to showering and accidental bumps. The sensor is water-resistant up to 2.4 meters/8 feet. The G7’s sensor connects directly to your smartphone as well, as long as it is within 20 feet of the sensor, updating at five minute intervals as opposed to every minute like the Libre. For technical clarity, it should be noted that both devices’ sensors are actually sensor and transmitter built into one unit. Unlike the products from Medtronic and Eversense.
Both sensor/transmitter units are compatible with both Android and iOS, but only the G7 is compatible with Apple Watch and some Android smartwatches. And for me, that’s actually a huge selling point. More on that in a bit.
Apps, Blood Glucose Timelines and Trends
Now that you know about the hardware, let’s talk about these CGMs and their respective apps. We know they’re sending data, but what features are you getting in those apps, and how easy is that data to understand and act upon?

Both apps show you a timeline of your readings for the day. The Libre 3’s home screen shows you a graph of the last 12 hours, and time remaining until your sensor ends, along with the current reading, and the status of your alarms. The G7 presents a card-based home screen anchored by a large bubble at the top which shows your current blood glucose reading with an arrow which tells you which way your blood glucose is trending, up/down/up rapidly/down rapidly. The first card shows your readings on a timeline graph like the Libre, but right from there you can choose to view that graphed data for the last 3, 6, 12, or 24 hours. And you can even get granular by touching and holding on the little dots/data points, which allows you to see the exact time of that reading and blood glucose level. You can’t do that with Libre’s timeline.
The G7 app is more refined, easier to navigate overall.
You can also tap the three dots in the upper right of that card and change your high (hyperglycemia) and low (hypoglycemia) alerts, as well as activate timed Quiet Modes. And below that you get a second card, the new integration with the Clarity app. This allows you to see your average glucose over the last 3, 7, 14, 30, or 90 days. You’ll also get a bar graph below that number which shows you the time in range spent for the multi-day segment you’ve selected. By my doctor’s suggestion, and unlike the international standard of 70-180 mg/dl, I have my range set to 80-130 in the Libre 3 app and in the separate Clarity app for Dexcom’s G7. The G7 app, however, does not allow you to set custom ranges in that initial today view on the home screen. It is locked to the international standard.
Both apps allow you to run more granular reports, as well as see charts of your daily trends, which are very helpful in tracking when and why your blood glucose elevates over time. They’ll both give you a glucose management indicator (GMI) as well. GMI is supposed to be representative of what a lab’s A1C number may be when you get blood work done, BUT your GMI could be higher or lower than a lab’s official blood work. For the G7, that GMI number is actually on the second card on the home screen. For the Libre 3 app, you’ll have to tap the hamburger menu to access that information.
And that really exemplifies the difference between the two devices’ apps. The G7 app is more refined, easier to navigate overall. You can get all of your reports in one app with the Libre 3, whereas you’ll have to open Dexcom’s separate Clarity app to run reports. But if I had to pick one it would be the G7’s app for how it presents info and how easy it is to interact with it. One big caveat with the G7 is that they’re still testing the app with Apple’s latest iOS software so there may be some bugs.
There were a couple times during the ten days where my reading was way off from the Libre 3. One morning, for example, my BG at one point was 67 while sleeping whereas the Libre 3 had me at 93. Given my history, I’m more inclined to believe the Libre 3 had the accurate measure and I wasn’t awake at that point to do a finger poke test to verify the readings. But that could also be the result of me being a side sleeper and the sensor being on the back of my right arm, which is usually underneath my head and the pillow. Excessive pressure on a CGM like that from my head and pillow on top of it for hours can throw off readings. And that is one last caveat with both apps. All CGMs I’m aware of today come with a disclaimer that you should use the old tried and true finger poke test to verify readings if your numbers seem off, either too high or too low. And some CGMs actually require you to do finger poke tests while wearing their product to calibrate the CGM.
Monitor Blood Glucose on Apple Watch
Cost being the same, the G7 has some advantages over the Libre 3 for Apple users which are well worth considering. In the world of health, two very important Apple integrations: Apple Health and WatchOS connectivity.
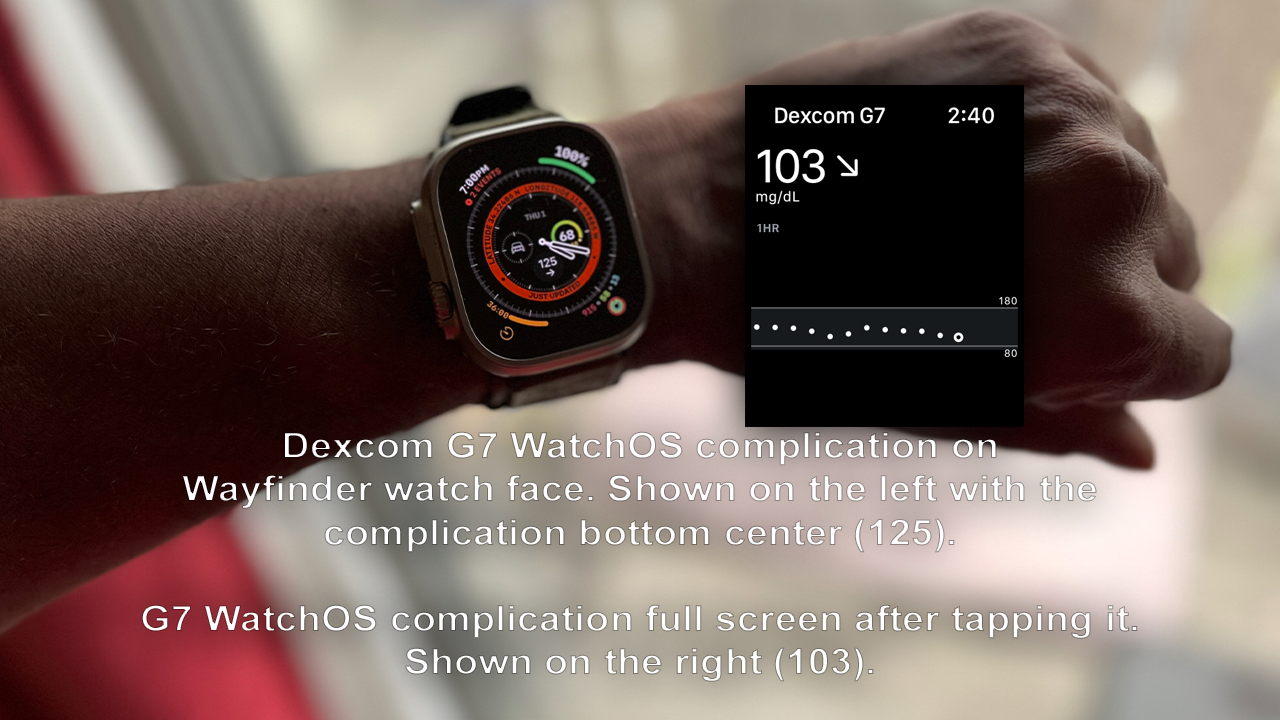
This for me is the most game-changing part of CGM use. For Apple smartwatch products, you get a WatchOS complication tied into the G7 iOS app. It doesn’t work without the phone but being able to see glanceable BG statuses on a complication throughout my day is a powerful “in your face reminder” which helps me stay on track and in some cases see how a food I didn’t think would raise my blood sugar actually does. Like grapes for instance. For me, grapes are a rocketship to hyperglycemia. Wearing the Libre 2 showed me that a while back but I had to wait for a high alert to hit my phone. The G7 app’s complication goes slightly beyond being just a complication by tapping on it and showing you your BG timeline. It will present you with the option to show the last 1, 3, or 6 hours of BG history when you tap on the timeline.
Dexcom tells me that direct Bluetooth connectivity between their sensors and Apple Watch is a feature they’re working towards.
The only caveat with the WatchOS complication is that WatchOS WidgetKit has a limitation on complication refreshes in a 24-hour period and Dexcom CGMs can provide as many as 288 glucose readings per day, exceeding that limit. So, from time to time I’ll see “—” instead of a reading when there isn’t a recent value to display. Once I tap the complication though, the data shows in the full screen applet and when I exit out, it’s right back there on the complication.
Apple Health Integration Brings It Home
Apple Health integration adds even more functionality to BG reporting. With the G7 data pumping through Apple Health, you’ll be able to see some very important data summaries, among other things.
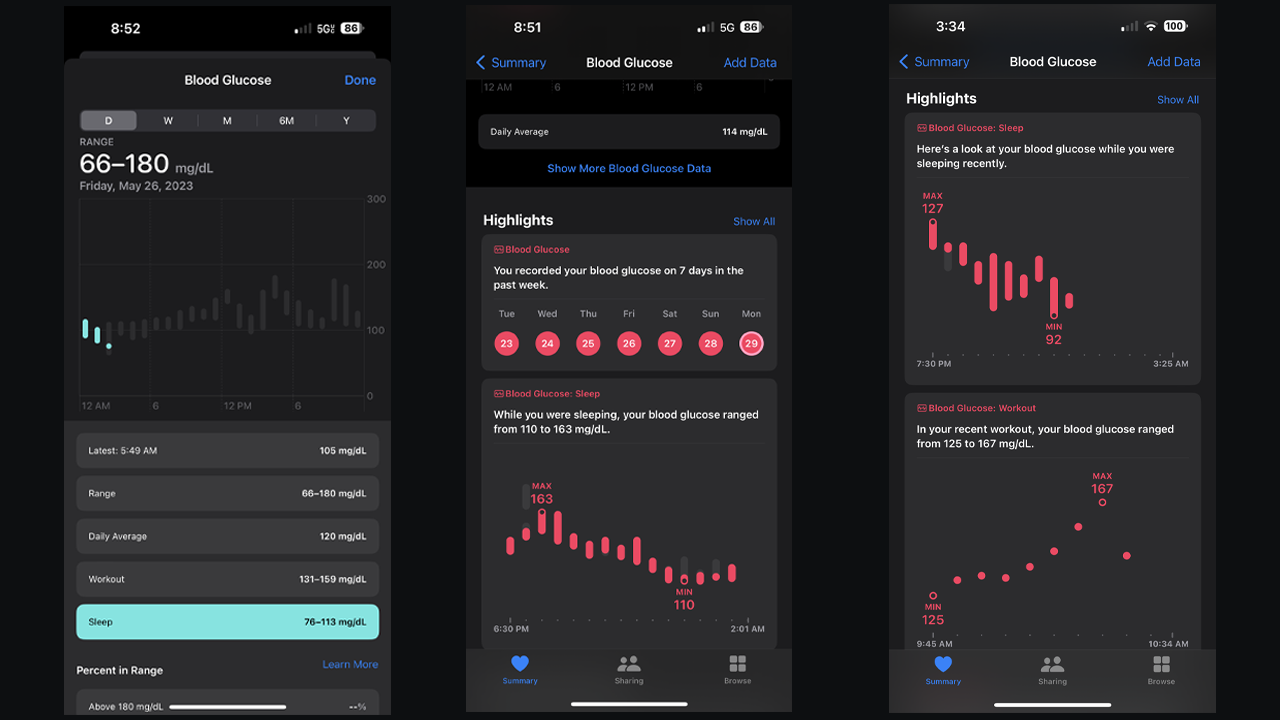
My favorite two are the Workout and Sleep summaries. They’re exactly what you think. You can see a summary of your BG levels during your sleep time logged from your devices. And you’ll be able to get a similar summary for the time you log a workout. Someone once said that the best medicine for a Type 2 diabetic is walking, and using the G7 and Apple Health I can see how my BG levels dip when I walk, or even run, as opposed to how they climb when I’m lifting heavy on strength training days. There’s a scientific reason for this, based on how your body utilizes sugar differently between cardio and strength training, especially heavy lifting. There are more blood glucose metrics you can dig through in Apple Health.
Protip: Despite your diabetes, never skip leg day.
Cost complications
When you’re first diagnosed, even with all of the amazing resources and message boards on the web, so much of your new life will be trial and error.
One final note as we bring things to a close in this look at both devices. As cost is hard to add to this deep dive because of how different insurances will handle your doctor’s prescription for these newer CGMs, it’s hard for me to relay those specifics to you. I was paying roughly $38 USD every 14 days for the Libre 2, so roughly $76 USD a month. I haven’t tried to update my prescription to the Libre 3 or the Dexcom G7 yet so I don’t know the costs for me. When my doctor first prescribed the Libre 2, he did so over the Dexcom G6, saying it was the cheaper option with my insurance. Abbott currently has a promotion on their Freestyle Libre website where you can try one 14 day sensor for free with a voucher if you are eligible. Dexcom reps tell me that the majority of patients with pharmacy coverage are paying less than $40 per month and that “Dexcom is currently reimbursed by 97% of private insurance as well as Medicare nationwide and Medicaid in 45 states.”
If the costs are fairly close for you, I’d highly recommend Dexcom’s G7 over the Libre 3. It’s connectivity with the Apple ecosystem sets it well beyond the functionality of the Libre 3 and gives it greater utility in the life of an Apple user.
With that said, no matter which device your insurance will cover, or that your budget will allow for, EITHER ONE is an absolute game changer for most diabetics, especially those in the Apple ecosystem and those newly diagnosed. When you’re first diagnosed, even with all of the amazing resources and message boards on the web, so much of your new life will be trial and error. But, the info a continuous glucose monitor provides is absolutely priceless in figuring out your new lifestyle and how your relationship with food needs to change in order for you to live a long, healthy life with this insidious disease.
